So you’ve probably noticed this at some point: two people taking the same medication for the same condition but both experience very different effects. One gets better quickly with no side effects, but the other doesn’t get better at all and faces severe reactions. That can’t make sense, right? It’s the same medication, so how could it result it two completely different results? Turns out, your genetic makeup not only tells your body your blood type, eye colour and other factors (genetic variations) but it also influences the way it responds to medicine. This is the field of pharmacogenomics.
What is Pharmacogenomics?
Let’s look at this linguistically. Pharmaco- means pharmacology, which is the science and understanding of drugs. -genomics means genomics (who would’ve guessed?), which is the study of genes. So pharmacogenomics is the understanding of how genes and DNA affect drugs!
More specifically, how variations in DNA can affect drug efficacy (how well the drug actually does its job) and drug safety (whether the drug will make you better with no side effects, or extreme side effects…) among human beings. Every person has a completely unique genetic code. That’s why every person you look at is different, even if it is slight. These genetic differences can impact how drugs are absorbed, metabolised, and ultimately removed by the body.
So why do we study this?
The creation of personalised medicine. An ideal future would be one where everyone can receive medicine that is personalised for them, so recovery is as fast as possible, and side effects are as minimal as possible. And clearly, pharmacogenomics has a huge role to play in that. It aims to be able to tailor drug therapies to individual patients to improve the recovery, reaching personalised medicine.
Why do Genes Affect Drug Response?
So at first glance, you might be asking exactly what genes have to do with drug response.
Our bodies rely on enzymes (biological catalysts made of protein) and other proteins to process drugs. They are produced using ribosomes, which are located in the cell and are responsible for reading DNA and transcribing it into instructions for creating proteins (protein synthesis) and enzymes. And as we already know, variations or mutations are extremely common, and that affects what the ribosome reads, resulting in an enzyme that is different. And ultimately, that means there are differences in how the drugs are handled.
Specifically, some people may have genetic variants the reduce enzyme function, causing drugs to build up in the body, maybe even causing toxicity. Others have variants that increase enzyme activity, breaking down drugs to quickly and making medications less effective.
Examples of Pharmacogenomic Impact
Now we know why genes affect drugs, but in practice, the majority aren’t affected too badly by differences in drug response. But still, pharmacogenomics is very important. These three drugs are the most common medicines with clear pharamacogenomic impact:
Warfarin
This a common blood thinner, used to prevent or treat blood clotting. Genetic differences in two enzymes (CYP2C9 and VKORC1) can affect dosing requirements. Too much could mean internal bleeding and inability to heal, and too little means that blood clots are still a risk.
Codeine
The enzyme CYP2D6 can convert codeine to its active form morphine. Ultra-rapid metabolisers can experience too much morphine, risking overdose, and poor metabolisers won’t experience a lot of pain relief.
Clopidogrel (Plavix)
This is an antiplatelet drug that is activated by CYP2C19. If your genetic makeup causes this enzyme to not be synthesised as much or not as efficiently, then you won’t benefit fully and you’ll need an alternative treatment.
How do Pharmacogenomic Tests Work?
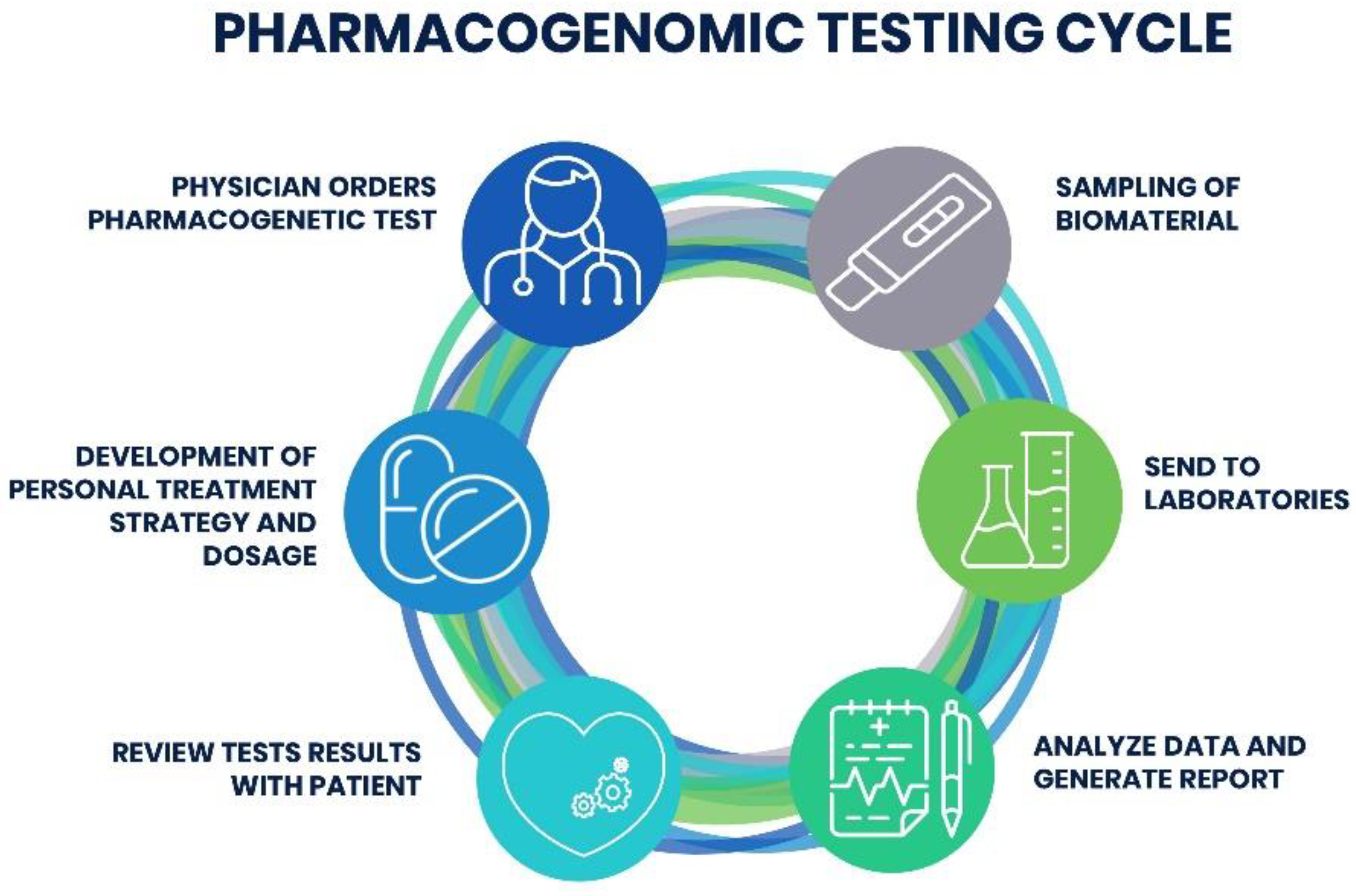
Given the importance of tailoring drugs to different patients based on their genes, it makes sense that there are tests to check specific genes that could affect the drug’s efficacy or safety.
Usually, it only involves a simple blood or saliva sample, to analyse the related genes. The results will provide guidance on which drugs and dosages might be safest and the most effective.
Especially recently, pharmacogenomic testing is becoming much more common in clinical practice, particularly when using medications with known major genetic interactions, or in cases where patients have has unexpected reactions.
Pharmacogenomics and the Future
Pharmacogenomic testing is expensive; self-kits cost £299 in the UK (https://fgih.co.uk/product/pharmacogenomics-test/)! So it’s understandable but annoying that they aren’t a huge priority in clinical practice. When technology advances and costs fall (as Moore’s Law states), genetic testing might become a routine part of medical care! Allowing doctors to choose the right drug and dose the first time and minimising severe drug reactions.
So there you have it, a short discussion on pharmacogenomics. Did you find this article helpful? What do you find most interesting about pharmacogenomics and its future? Let us know in the comments. Thanks for reading!
Written by Hamd Waseem (14)